Hospitals: Know Your Pharmacy Board

This is not a case of ‘what you don’t know won’t hurt you’. Pharmacy boards use regulations to interfere with competitor operations. Boards dominated by independent pharmacy owners try to restrict chain drug stores. Chain drug store boards look to interfere with independents and hospital outpatient pharmacies.
Pharmacy regulations are meant to ensure the safety of patients. But what happens if those regulations also impose operating restrictions that determine who can effectively compete for patients, or even interfere with patient-centric innovation? For hospitals, this should be a big concern.
Only 15% of State Board of Pharmacy members are hospital pharmacists and few of those members identify practical experience with outpatient pharmacy operations. 25% of state pharmacy boards do not include a hospital pharmacist. This places hospitals at a significant disadvantage when new technologies emerge that could benefit hospital patients, or if hospital operations preclude the possibility of errors or abuse found in traditional retail pharmacy.
Why is this important? Retail bias interferes with hospital efforts to improve therapeutic outcome and provide patients with better pharmacy services. Apart from this, retail bias in regulations may violate the Sherman Anti-Trust Act, interfere with innovation and adoption of new technology.
Consider the Illinois State Board of Pharmacy dominated by a major drug chain. Pharmacy regulation Section 1330.680 d), specific to hospitals, restricts outpatient pharmacies to operate in the same manner as retailers in the application of technology. This operations overreach by the Board restricts outpatient operations from leveraging pharmacist staff and fully utilizing available dispensing technologies.
Like Illinois, North Carolina State Board of Pharmacy does not include hospital pharmacists. Four of the six members are retail independents and two are public members. Regulations favor independents with restrictions on technology and remote drive-thru location (although retailers seem to ignore the latter). This regulation overreach prevents hospitals from serving multiple patient discharge points despite an abundance of patient contact with a clinical pharmacist and more thorough medication review than provided by retailers.
Things Hospitals Should Look For in Pharmacy Regulations
It is in the interest of drug retailers looking to expand ambulatory pharmacy business to restrict hospital outpatient pharmacy operations to function as retail clones, denying hospitals (and patients) benefits realizable with superior health care and pharmacy infrastructures. Point-of-care prescription access is the holy grail for retail … but only on their terms.
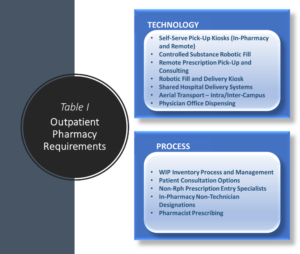
Pharmacy regulations should ensure patient safety and avoid interfering with technology and process that enhance safety and outcome. Table I lists requirements for effective outpatient pharmacies, and hospitals should ensure regulations do not prevent or restrict these in their pharmacy.
Technologies exist that allow the controlled hospital environment to address patient therapeutic outcome challenges and reduce patient discharge-to-home transition risks. These same technologies would improve patient care in retail operations but are cost prohibitive for most retailers to implement.
Hospitals can provide the special footprint and processes retailers are unwilling, and retail bias in pharmacy regulations should not prevent them from effectively serving urgent markets. Retail on-demand fill process would change significantly to effectively serve urgent markets. As was the case with technology, retail could address the special needs of urgent markets but at a cost to profit.
Things Hospitals Should Require for Retail Regulation
With only 15% hospital representation on state pharmacy boards, it is fair to say that regulations have a retail bias. This bias can result in prohibitions or allowances that increase the risk patients bear in prescription delivery. Insulated from the risks of unfavorable therapeutic outcome or ADE, retailers benefit from regulations that do not require pro-active pharmacist interaction with patients and prescribers.

Table II identifies patient-centric therapeutic outcome requirements regulators should require for retailers. These regulations would require retailers to ensure accurate DUR, patient understanding of medication use and side effects, and address non-compliance by closing the prescriber-patient-prescription delivery loop.
Hospitals offer the only true competition for retail pharmacies and have a vested interest to improve therapeutic outcome. Outpatient pharmacy operations need to be transformative, adopt new technologies and leverage assets of the hospital. For this to happen, they must work together to eliminate retail bias in pharmacy regulations … and that begins with a seat at the table.
Note: ‘Boardroom’ art sourced from youwall.com.